Burn injuries account for over 100,000 hospital admissions per year. With the opening of many specialized burn centers for acute burn injuries, death rates from severe burns have dropped significantly. Survivors, however, are often left, with functional impairment and grotesque distortion of appearance. Particularly is located in the head and neck regions. Functional impairment in the head and neck region results in drooling, neck contracture, corneal exposure, nasal airway blockage, lip incompetence, inability to make facial expressions, etc. As a specialist in reconstruction and burn rehabilitation, the plastic surgeon is an integral part of the burn team. Scarring, whether it's normal or hypertrophic, contractures, loss of functional body parts, and change in the color and texture of burned skin are processes common to all burned patients that have the potential to be reconstructed.
A realistic approach, however, is necessary to harmonize patients' expectations (which are often very high) with the likely outcomes of reconstructive surgery. Burn reconstruction starts when a patient is admitted with acute burns and lasts until the patient's expectations have been reached or there is nothing else to offer. However, even when this time has come, the patient-surgeon relationship may still continue and can last a lifetime.
What are the reconstructive options?
As with the initial treatment of severe burns, reconstructive burn procedures often require skin grafting or flap reconstruction. Skin grafts involve taking skin from unburned sites on the body (known as donor sites). This skin is then placed (grafted) onto the burn wound. The grafted skin attaches to the underlying wound and effectively closes it.
Skin grafts are often used in the revision of scar contracture, which is another unfortunate consequence of burns. A contracture is a permanent shortening of the muscle, tendon or scar tissue producing deformity or distortion. Contractures often restrict normal body movement. In these reconstruction procedures, a surgeon excises (removes) an existing scar and applies a graft to the site of the removed scar. Skin grafting for burn reconstruction is a surgical procedure and is usually performed in the hospital on an inpatient basis under general anesthesia. As with grafts used for initial treatment, recovery may take several weeks.
A graft "takes" or is successful when new blood vessels and tissue form in the injured area. Sometimes, skin grafts do not take because of early complications such as infection (the most common cause of graft failure), shearing (mechanical forces that cause a graft to detach from the skin), or fluid collections underneath the graft. While grafting is a proven and effective treatment, it is important to understand that all grafts leave some scarring at both the donor and recipient sites. More Burn Surgery Facts...
-
Split-Thickness GraftsSplit-thickness skin grafts (STSGs) are grafts that include the thin top layer of the skin (epidermal layer) and part of the underlying thicker component of skin (dermal layer). Split thickness skin grafts are often removed from flat body surfaces such as the abdomen, thigh or back. These grafts are sewn or stapled into place on the wound/burn and covered with compression dressings (tightly wrapped elastic bandages) to provide firm contact. Occasionally, graft sites are left open to air.
Split-thickness skin grafts are generally not used for weight-bearing parts of the body or for areas subject to friction such as hands or feet. The advantages of STSGs include less tissue use, an improved chance of graft survival and minimized donor site damage. However, one disadvantage is that these grafts tend to contract more than full-thickness skin grafts. More Burn Surgery Facts... -
Full-Thickness GraftsFull-thickness skin grafts (FTSGs) consist of both the epidermal and complete dermal skin layers. This type of graft is used instead of a split-thickness skin graft when cosmetic outcome is essential and contracture is not tolerable for function. The thicker the graft, the less the potential there is for contracture. Other advantages include increased resistance to trauma over thin grafts and less distortion functionally and cosmetically. More Burn Surgery Facts...
-
Skin FlapsSometimes, the area requiring reconstruction lacks the blood supply needed to support a skin graft. Skin flaps, an advanced form of skin grafting, is a complex procedure in which skin, along with underlying fat, blood vessels and sometimes muscle, is moved from a healthy part of the body to the injured site. In skin flaps located adjacent to the wound site, blood supply may remain attached at the donor site. In instances where the skin flap needs to be attached to a wound elsewhere on the body, surgeons will reattach blood vessels in the flap at the new site through microvascular surgery. More Burn Surgery Facts...
-
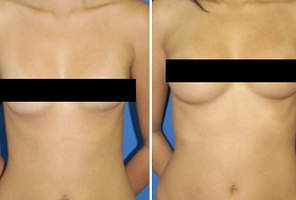
Tissue ExpansionTissue expansion is an important and valuable addition to the reconstructive armamentarium of plastic and reconstructive surgeons. It is a safe technique and can be used successfully for the rehabilitation of selected burn victims. It allows the creation of skin that maintains all the skin characteristics in the area (sensation, texture, color, and hair follicles) with minimal or no donor site complications.
At the time of tissue expander placement, a moderate volume of saline is placed, but only enough to fill the space without too much tension on the suture line. Inflation schedules must be individualized according to the nature and location of the deformity. Filling is generally performed at weekly intervals, and each inflation proceeds to a point of slight discomfort or blanching of the skin overlying the implant.
After making the decision to use tissue expansion, the surgeon must choose the type of flap to be used. When the desired expansion has been achieved, the expander is removed and the flap is moved to the recipient site.
Patient selection is very important, since this process implies a temporary but significant cosmetic deformity and may interfere with social life and other activities. Only well-motivated persons should be considered as candidates for the procedure, following extensive pre-surgery discussion. More Burn Surgery Facts... -
Donor SitesWhen performing a skin graft, the surgical team must pay attention to the donor site as well since that can also result in poorly healed tissue. Thick split-thickness and full-thickness skin grafts result in deeper donor site wounds that require longer healing time and may result in contraction and hypertrophic scarring.
With thicker split-thickness and full-thickness skin grafts, dermal tissue may be permanently lost at the donor site. The dermal layer cannot grow back by itself and most often results in scar formation. Healing time for most split-thickness skin grafts is approximately 10 to 20 days. Most full-thickness skin grafts require a longer 21 to 90 day period. As a result, medium-thickness split grafts are frequently used as a compromise to provide improved graft survival and durability with minimized donor site complications. More Burn Surgery Facts...
How do surgeons decide what to use?
In evaluating your condition, a plastic surgeon will be guided by a set of rules known as the reconstructive ladder. The least-complex types of treatments-such as simple wound closure-are at the lower part of the ladder. Any highly complex procedure-like micro-surgery would occupy one of the ladder's highest rungs. A plastic surgeon will almost always begin at the bottom of the reconstructive ladder in deciding how to approach a patient's treatment, favoring the most direct, and least-complex way of achieving the desired result.
The size, nature and extent of the injury or deformity will determine what treatment option is chosen and how quickly the surgery will be performed. Reconstructive surgery frequently demands complex planning and may require a number of procedures done in stages.
Everyone heals at a different rate-and plastic surgeons cannot pinpoint an exact "back-to-normal" date following surgery. They can, however, give you a general idea of when you can expect to notice improvement. More Burn Surgery Facts...
What are the risks and concerns about Burn reconstruction?
As with any surgery, complications can occur. Individuals vary greatly in their anatomy and healing ability and the outcome is never completely predictable. Complications include infection; excessive bleeding, such as hematomas (pooling of blood beneath the skin); significant bruising and wound-healing difficulties (hypertrophic scarring and keloid formation); and problems related to anesthesia and surgery. Once again, it is always important to be realistic in your expectations and to have good communication with your plastic surgeon regarding the possible outcome.
In general, a patient is considered to be a higher risk if he or she is a smoker; has a connective-tissue disease; has areas of damaged skin from radiation therapy; has decreased circulation to the surgical area; has HIV or an impaired immune system; or has poor nutrition. More Burn Surgery Facts...
Disclaimer:
This information is intended only as an introduction to this procedure. This information should not be used to determine whether you will have the procedure performed nor does it guarantee results of your elective surgery. Further details regarding surgical standards and procedures should be discussed with your physician.